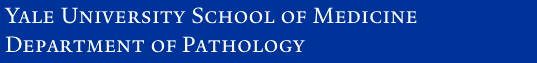
The blood smear shows schistocytes, which are fragmented, deformed, irregular, or helmet-shaped RBCs. Schistocytes are the result of the partial destruction of RBCs that occurs as they traverse vessels partially occluded by microthrombi.
This patient has Hemolytic Uremic Syndrome (HUS) caused by infection with E. coli O157:H7, following ingestion of undercooked meat or by exposure to the fecal material from infected animals. This bacteria produces a Shiga-like toxin that preferentially attacks the microvessels in the kidney and intestines. This damage, in turn, causes the endothelium to increase its expression of von-Willebrand factor, causing platelet aggregation and thrombosis. The thrombi are principally composed of platelets, which means that the PT and PTT times (which measure fibrinolysis) are generally normal.
HUS is closely related to another disease called Thrombotic Thrombocytopenic Purpura (TTP). In TTP, there is an inherited (genetic) or acquired (autoimmune antibody-mediated) deficiency of a plasma enzyme called ADAMTS13. ADAMTS13 degrades multimers of von Willebrand factor (vWF), and in its absence vWF accumulates, promoting platelet activation and aggregation. This will be covered in detail next year.
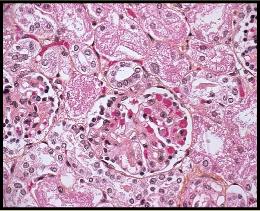
In this patient, the damage to the intestines resulted in perforation, peritonitis, and sepsis. A complication of sepsis is Disseminated Intravascular Coagulation (DIC). In DIC, the systemic release of inflammatory cytokines increases vascular permeability, increases blood viscosity, causes vasodilation, and activates Factor VII, complement and endothelial cells. The result is the development of numerous microthrombi. In contrast to the thrombi seen in HUS, those of DIC contain both platelets and lots of fibrin. In fact, the consumption of fibrin and platelets in these microthrombi causes a paradoxical hypocoagulable state leading to hemorrhage (petechiae and ecchymoses). DIC thrombi can occur anywhere, but are frequently seen in the brain, heart, lungs and kidney.
This 2010 New York Times article tells the story of a patient misdiagnosed with HUS/TTP instead of malignant hypertension.
You see an 8-year old boy with bloody diarrhea, hypertension, and oliguria. His history is significant for a recent trip to a petting zoo where he ate a hamburger.
Blood analysis demonstrates a mild thrombocytopenia and anemia, though PT and PTT levels are normal. A smear of the patient's blood is shown here.
How would you characterize the pathology?
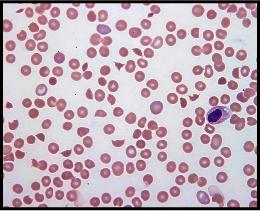
A kidney biopsy is performed to investigate the patient's declining renal function.
What do you see?
Does this fit with the blood smear above?
Does the clinical history tip you off to a much publicized disease? What is the disease caused by?
After a rocky hospital course, the patient develops sepsis and dies.
At autopsy you note diffuse petechial hemorrhages and ecchymoses on the skin.
Histologic analysis of the kidney after death is shown to the left along with a "special stain" for fibrin.
How does this fit with the patient's skin lesions?