
You proceed to serially section the heart, and identify a myocardial infarction at the site of the defect.
Of the two gross images, which do you think is more consistent with what you see in your patient?
Which is appears more acute, which appears chronic and why?
Why does the infarct on the left have central pallor and a hyperemic boarder?
Even patients that have survived a myocardial infarction (MI) for months can have a sudden death. What do you think a primary cause of death in such patients might be?
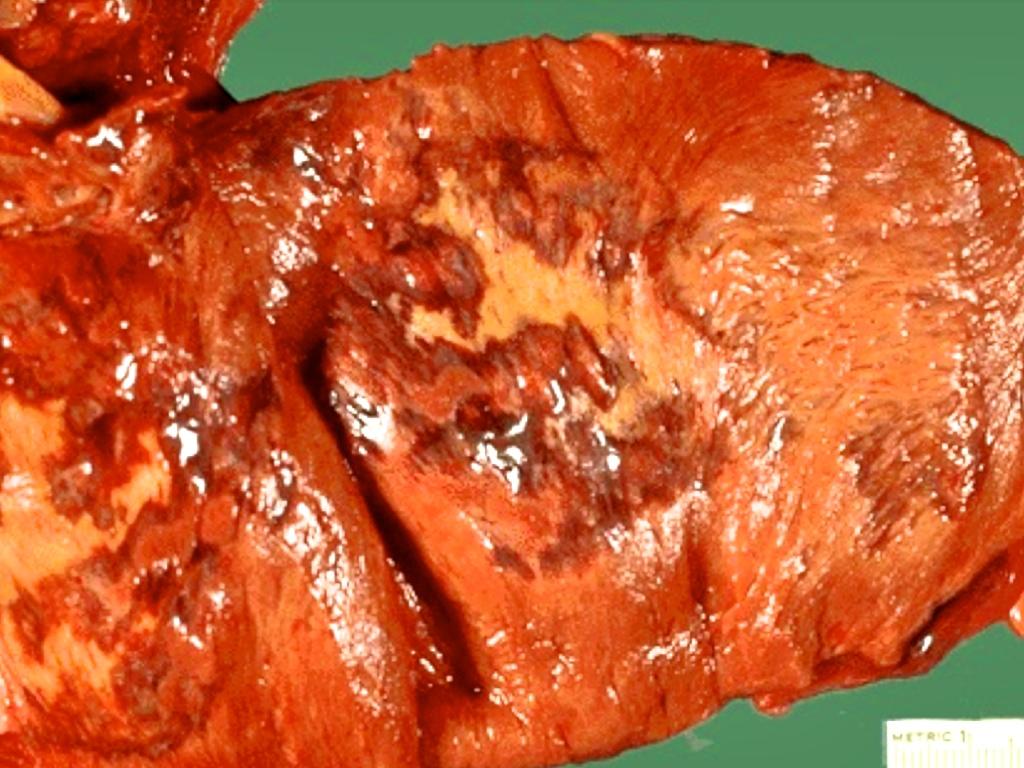
Initially, infarcts will appear as reddish-blue areas caused by the presence of stagnating, trapped blood cells. Over the next 7-14 days the infarct will become a more sharply defined area of yellow-tan softening rimmed by a hyperemic zone. This area of hyperemia represents the formation of vascularized granulation tissue.
Cardiac tamponade occurs in recent infarcts (5-7 days) at the peak of tissue softening (necrosis) but prior to fibrosis.
Cardiac tissue does not regenerate and the tissue is replaced by fibrous tissue as the final event of the inflammatory response. This process can take months. The gross appearance of these "old" or "remote" infarcts are white and fibrous (right image).
Fibrosis in the myocardium reduces the risk for tamponade, but maintains the risk for disrupting the conduction system of the heart. This can place patients into a cardiac arrhythmia causing sudden death. Large fibrotic areas are not contractile and decrease cardiac output. They also provide an area of disrupted flow (remember Virchow's triad) that predisposes patients to the development of intracardiac thrombi.